Published by: Biju Murali, Sundeep Vijayaraghavan, P. Kishore, Subramania Iyer, Mathew Jimmy, Mohit Sharma, George Paul, Sachin Chavare (Department of Plastic and Reconstructive Surgery, Amrita Institute of Medical Sciences, Kochi, India)
Published in: Indian Journal of Plastic Surgery January-April 2011 Vol 44 Issue 1
Address for correspondence: Dr. Biju Murali, Department of Plastic and Reconstructive Surgery, Amrita Institute of Medical Sciences, Kochi, India. E-mail: biju_daks2000@yahoo.com
ABSTRACT
Background: Gynecomastia is usually treated with liposuction or liposuction with excision of the glandular tissue. The type of surgery chosen depends on the grade of the condition.
Objective: Because gynecomastia is treated primarily as a cosmetic procedure, we aimed at reducing the invasiveness of the surgery.
Materials and Methods: The technique complies with all recommended protocols for different grades of gynecomastia. It uses liposuction, gland excision, or both, leaving only minimal post-operative scars. The use of cross-chest liposuction through incisions on the edge of the areola helps to get rid of all the fat under the areola without an additional scar as in the conventional method.
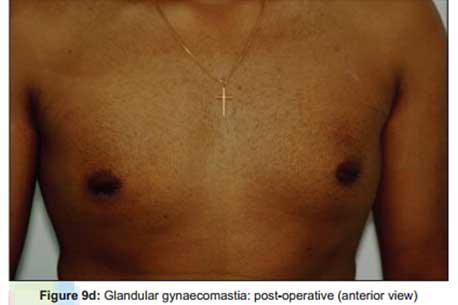
Results: This is a short series of 20 patients, all with bilateral gynecomastia (i.e., 40 breasts), belonging to Simon’s Stage 1 and 2, studied over a period of 2 years. The average period of follow-up was 15 months. Post-operative complications were reported in only two cases, with none showing long-term complications or issues specifically due to the procedure.
Conclusions : Cross-chest liposuction for gynecomastia is a simple yet effective surgical tool in bilateral gynecomastia treatment to decrease the post-operative scars. The use of techniques like incision line drain placement and post-drain removal suturing of wounds aid in decreasing the scar.
INTRODUCTION
Gynecomastia is a common condition for which a medical intervention is sought. Liposuction with or without gland excision is the commonly used technique among plastic surgeons. The procedure chosen is determined by the grade of the condition. Conventionally, liposuction in gynecomastia is performed using one or two small incisions on each side of the chest.

The gland is excised through a periareolar incision. This is followed by the insertion of drains either through one of the liposuction entry wounds or through a separate incision. The drain site and liposuction wounds are not sutured and are left to heal secondarily, leading to visible scars in the chest in addition to the periareolar wounds. But, when the liposuction is performed through incisions in the periareolar region, the fat below the areola cannot be addressed satisfactorily, which may necessitate the use of larger incisions to deliver the gland.
The gland is excised through a periareolar incision. This is followed by the insertion of drains either through one of the liposuction entry wounds or through a separate incision. The drain site and liposuction wounds are not sutured and are left to heal secondarily, leading to visible scars in the chest in addition to the periareolar wounds. But, when the liposuction is performed through incisions in the periareolar region, the fat below the areola cannot be addressed satisfactorily, which may necessitate the use of larger incisions to deliver the gland.
MATERIALS AND METHODS
Technique
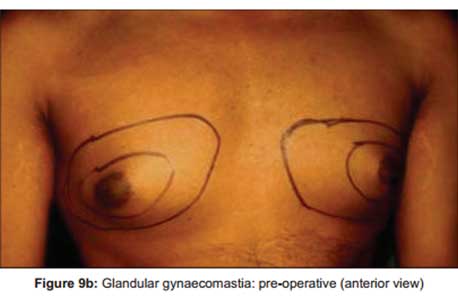
The markings are performed in an upright posture and general anesthesia is administered. The patient is positioned supine on the table. The breast is infiltrated with 200–250 ml of tumescent fluid (1 L Ringer lactate with 20 ml of 2% lignocaine, 20ml sodium bicarbonate, 1 ml of 1:1000 adrenaline and 1500 IU hayaluronidase added to it).
The initial incision for liposuction is a 7-mm stab made at the 6’o clock position at the skin–areola junction of the nipple areola complex.

Pre-tunneling before liposuction is carried out using a liposuction cannula through this incision. A 3-mm-diameter liposuction-cannula with the Mercedes Benz tip is inserted and liposuction of the ipsilateral breast is completed.

The same procedure is repeated on the opposite breast as well. All liposuctions were carried out using a power-assisted device.
At the end of this step of liposuction, the sub-areolar part of both the breasts remains unaddressed. A 4-mm-diameter liposuction cannula is inserted through the same incisions and liposuction of the sub-areolar regions of the opposite breasts is also performed after creating one tunnel across the chest.

Then, through another tunnel, the inframammary area is again sucked. Care is taken to stick to only two tunnels across the chest wall to prevent synmastia. The liposuction is done in such a way that there is a 5-mmthick layer of fat that is left underneath the skin at all the regions. The volume of fat aspirated from each side is noted.
In patients requiring a glandular excision, the stab incision is extended for 2 mm on either side into a periareolar incision and the glandular elements are removed surgically.

Post-operatively, a suction drain is inserted and brought out through the same incision. The wound is closed in two layers. Half-buried vertical mattress sutures are used so that there are no marks on the skin side of the incision. A mattress suture is placed and left loose in the part of the incision through which the drain is passed, to be tied later after removal of the drain. This was followed by pressure vest from the immediate post-operative period, the dressings were changed on the first or second postoperative day and the drains were removed when the drain volume was <30 ml. The patients were discharged on the same day of the procedure. This was followed by regular clinical follow-up at 3 months, 6 months, 18 months and 24 months.

This was followed by pressure vest from the immediate post-operative period, the dressings were changed on the first or second postoperative day and the drains were removed when the drain volume was <30 ml. The patients were discharged on the same day of the procedure. This was followed by regular clinical follow-up at 3 months, 6 months, 18 months and 24 months.
Study
The study was conducted at the Institute during the period from March 2008 to April 2010. The total number of subjects enrolled in the study was 20. All the patients underwent a clinical and hormonal screening for physiological, pharmacological and various pathological causes.
All the cases included in the study were of idiopathic etiology. The patients belonged to the age group ranging from 14 years to 52 years (mean age, 33 years). All the subjects sought medical help for cosmetic reasons. All cases included in the study belonged to Simon’s grade 1 and 2 and all cases requiring skin excision were excluded from the study.
The protocol followed was to use liposuction alone in Simon’s grade 1 and fat-predominant grade 2a patients and a combination of suction-assisted lipectomy and skin sparing adenectomy (glandular excision) in Simon’s grade 2b who do not require skin excision and gland-predominant grade 2a patients.
Twenty subjects were enrolled in the study. All subjects had bilateral gynecomastia. Thus, 40 individual breasts were studied. All fat-predominant breasts were treated with liposuction alone and the gland-predominant ones underwent liposuction and gland excision.
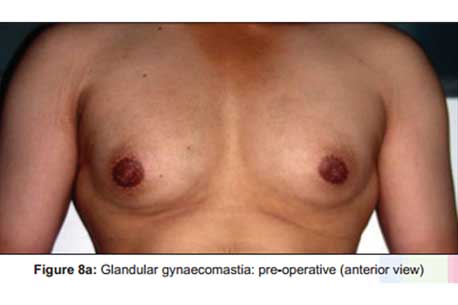





In eight (20%) breasts, liposuction alone was performed while the remaining breasts, i.e. 32 (80%), underwent liposuction and gland excision. Liposuction aimed to attain an even thickness of the panniculus over the anterior chest.


The follow-up period ranged from 3 months to 24 months (average of 13 months).
Complications were reported in two cases. Both the complications occurred in the unilateral breasts. One case developed a seroma and the other a haematoma. The seroma was aspirated and treated with antibiotics and compression. The haematoma was re-explored and the clots were evacuated and haemostasis was achieved. There was no incidence of recurrence, synmastia, hypertrophic scaring or any other complications specific for this procedure in any of the cases during the period of follow-up.
DISCUSSION
Gynaecomastia or overdevelopment of the male breast was a term first used by Galen in the 2nd century AD. Thirty percent of the middle aged and 60% of the adolescent boys have significant gynaecomastia.
The common treatment protocol is to perform liposuction alone for Simon’s grade 1 and fat-predominant type of grade 2a, liposuction with gland excision for gland predominant type 2a as well as 2b with good-quality skin.
Liposuction along with gland excision and skin excision is offered for grade 3 and for some cases of 2b.
The sub-areolar glandular excision is performed leaving a cuff of tissue 1–1.5-cm-thick under the skin. Liposuction is done leaving a layer of subcutaneous fat 5-mm-thick under the skin.
Conventionally, liposuction in gynaecomastia is done through an inframammary fold incision and lateral chest stab incisions. The drains are inserted through these liposuction wounds. These will result in small scars in the anterior and lateral chest, giving an “operated” appearance.
If liposuction is performed through a periareolar incision alone, adequate suction of the sub-areolar region is not possible, but this technique of “cross-liposuction” allows good suction at the sub-areolar region as well. The insertion of a drain through the incision site leaves no additional scar. Mattress sutures at the drain sites enable us to get a good post-operative scar. The use of half-buried, vertical mattress sutures leaves a hardly detectable scar on the skin. There is no additional morbidity associated with the technique of cross-chest liposuction.
REFERENCES
Braunstein GD. Clinical practice: Gynecomastia. N Engl J Med 2007;357:1229-37.
Rohrich RJ, Ha RY, Kenkel JM, Adams WP Jr. Classifcations and management of gynecomastia: Defning the role of ultrasound assisted liposuction. Plast Reconstr Surg 2003;111:909-23.
Simon BE, Hoffman S, Kahn S. Classifcation and surgical correction of gynecomastia. Plast Reconstr Surg 1973;51:48-52.
Deutinger M, Freilinger G. Gynecomastia: Attempt at a classifcation and surgical results. Handchir Mikrochir Plast Chir 1986;18:239-41.
Gasperoni C, Salgarello M, Gasperoni P. Technical refnements in the surgical treatment of gynecomastia. Ann Plast Surg 2000;44:455-8.
Webster JP. Mastectomy for gynecomastia through semicircular intraareolar incisions. Ann Surg 1946;124:557-75.
Voigt M, Walgenbach KJ, Andree C, Bannasch H, Looden Z, Stark GB. Minimally invasive surgical therapy of gynecomastia: Liposuction and exeresis technique. Chirurg 2001;72:1190-5.
Ohyama T, Takada A, Fujikawa M, Hosokawa K. Endoscope assisted transaxillary removal of glandular tissue in gynecomastia. Ann Plast Surg 1998;40:62-4.
Hammond DC, Arnold JF, Simon AM, Capraro PA. Combined use of ultrasonic liposuction with the pull-through technique for
the treatment of gynecomastia. Plast Reconstr Surg 2003:112: 891-5.
Maladick RA. Gynecomastia: Liposuction and excision. Clin Plast Surg 1991;18:815-22.
Persichetti P, Berloco M, Casadei RM, Marangi GF, Di Lella F, Nobili AM. Gynecomastia and the complete circumareolar
approach in surgical management of gynecomastia. Plast Reconstr Surg 2001;107:948-54.
Wiesman IM, Lehman JA Jr, Parker MG, Tantri MD, Wagner DS, Pedersen JC. Gynecomastia: An outcome analysis. Ann Plast Surg 2004;53:97-101.
Fruhstorfer BH, Malata CM. A systematic approach to surgical treatment of gynecomastia. Br J Plast Surg 2003;56:237-46.
Hamilton S, Gault D. The tuberous male breast. Br J Plast Surg 2003:56:295-300.
Johnson RE, Murad MH. Gynecomastia: Pathophysiology, evaluation and management. Mayo Clin Proc 2009;84:1010-5.

I’m really impressed with your writing skills as well as with the layout on your blog.
Is this a paid theme or did you modify it yourself? Anyway
keep up the nice quality writing, it is rare to see a great
blog like this one nowadays.
Thank you Mr Colmenero
Good afternoon. Great article.